
Disabilities &
Medical Conditions in Special Needs Adoption
Many children waiting for adoptive families have special needs, ranging from mild to significant.
Many children eligible for international adoption today have disabilities or medical conditions that require specialized care. While the prospect of parenting a child with special needs can seem intimidating, these conditions vary greatly — and are often less significant than an adoptive family may initially believe.
We encourage all prospective adoptive families to be open and honest throughout the adoption process, and learn more about the profile of child they are prepared to parent. Below, you will find important information about some of the more common disabilities and medical conditions among children waiting to be adopted. You’ll also find stories from experienced Holt families who are successfully caring for a child with one of these common conditions.
Index of Medical Conditions on This Page:
Autism
Autism, also known as autism spectrum disorder, is a developmental disorder that affects one in every 59 children. Boys are diagnosed with autism three to four times more frequently than girls.
Children with autism often have difficulties communicating or socializing with others. They can also exhibit repetitive behaviors or limited interests in activities.
Autism often begins before the age of 3 and can last throughout a person’s life, although symptoms may improve over time. Some children show symptoms of autism within the first year of life. In others, symptoms may not appear until 24 months or later. Some children with autism gain new skills and meet developmental milestones until they are 18-24 months of age. They then stop gaining new skills or lose the skills they once had.
Kids with autism can have a range of different symptoms and behaviors, so autism is considered a spectrum. For example, some children with autism may have advanced conversation skills, while others may be nonverbal. Some people with autism need a lot of help in their daily lives, whereas others can work and live with little to no support.
Autism affects each person differently, meaning that people with autism have unique strengths and challenges and different treatment needs. Treatment plans often seek to reduce symptoms that interfere with daily functioning and quality of life. They usually involve multiple professionals and are catered to the individual.

“I learn a lot from Tobin. One is that you should be patient and kind. Two is that you should treat him good, like hugging him. Three is that he shows me how to love and that everybody brings good into the world.”
— Knox Beard, brother of Tobin, who was diagnosed with autism
Attention-Deficit/Hyperactivity Disorder
Attention-Deficit/Hyperactivity Disorder (ADHD) is a developmental disorder associated with an ongoing pattern of inattention, hyperactivity and/or impulsivity.
Symptoms of ADHD can interfere with daily activities and relationships. ADHD begins in childhood and can continue into the teen years and adulthood.
Researchers are not sure what causes ADHD, although many studies suggest that genes play a large role. Like many other disorders, ADHD probably results from a combination of factors. In addition to genetics, researchers are looking at possible environmental factors that might raise the risk of developing ADHD and are studying how brain injuries, nutrition and social environments might also play a role.
Although there is no cure for ADHD, currently available treatments may help reduce symptoms and improve functioning. ADHD is commonly treated with medication, education or training, therapy or a combination of treatments.
Cerebral Palsy
Cerebral palsy is a disorder that impairs body movement, muscle tone and coordination. It is caused by brain damage before or during birth, or in the first 3 to 5 years of life.
Problems arise because of abnormalities in parts of the brain that control muscle movements, not the muscles themselves. Cerebral palsy can affect the body in different ways (right or left side, arms or legs, or both), depending on the severity of the disease.
The brain damage that leads to cerebral palsy can also lead to other health issues, including mental delays, seizures, vision, hearing and speech problems, and learning disabilities. The condition does not worsen over time. There is no cure for cerebral palsy, but treatment, therapy and special equipment can greatly improve a child’s capabilities.
The earlier treatment begins, the better chance a child has of overcoming developmental disabilities and learning new ways to accomplish daily tasks.

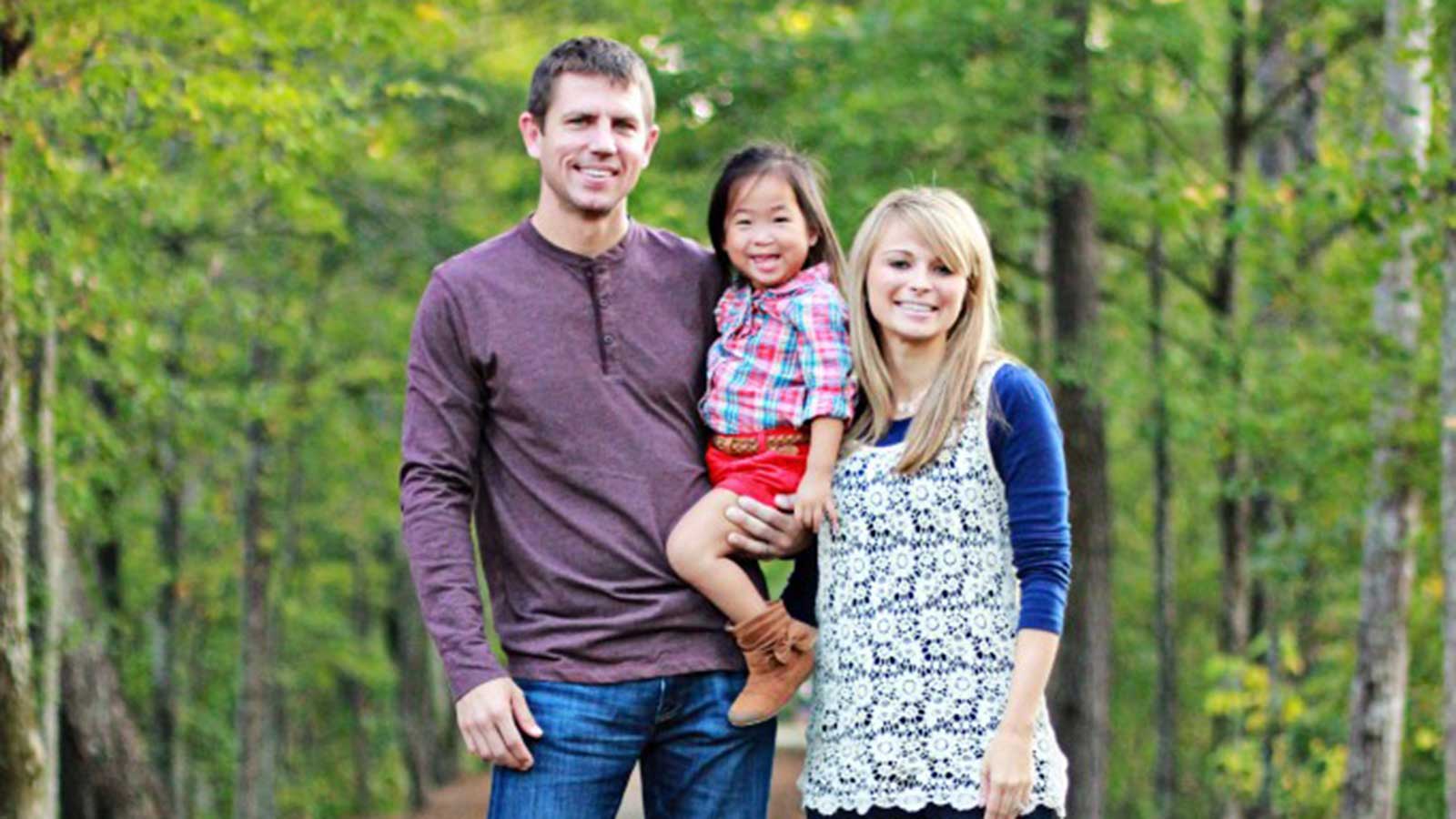
“There have been some little [ways in which] we’ve had to adapt to her — such as her not walking as fast — and we pick her up for long distances. But really, it hasn’t been that much of a shift in our thinking… We certainly didn’t have any trouble falling in love with her.”
— Drew Horine, father of Devki, who has cerebral palsy
Cleft Lip & Cleft Palate
Cleft lip and palate are birth defects that affect the upper lip and the roof of the mouth.
A cleft lip may be a small split in the lip or a complete split in the lip that goes all the way to the base of the nose. The cleft can occur on one or both sides of the lip. A cleft palate causes an opening in the roof of the mouth, or palate. It can occur on one or both sides of the palate, and extend for its full length. Cleft lip and cleft palate can occur together or separately.
Children with a cleft lip or palate often have problems with feeding and speaking clearly and can have ear infections. They might also have hearing problems and problems with their teeth. They will require surgery to correct the condition.
Surgery to repair a cleft lip usually occurs in the first few months of life and is recommended within the first 12 months. Surgery to repair a cleft palate is recommended within the first 18 months or earlier if possible. Many children will need additional surgical procedures as they get older.
Surgical repair can improve the look and appearance of a child’s face and might also improve breathing, hearing, and speech and language development. Children born with orofacial clefts might need other types of treatments and services, such as special dental or orthodontic care or speech therapy. With treatment and care, most children do well and lead a healthy life.
“[Hannah] is funny, smart, beautiful, bossy, and most importantly, ours. We love that when God knit her together, He knew that the very ‘disability’ that others would see would be what brought her together with her forever family.”
— Liz Barnette, mother of Hannah, who was born with a cleft lip and palate
Congenital Heart Disease
Congenital heart disease (CHD) is a problem that is present at birth and can affect the structure of a baby’s heart and the way it works. In some cases, the heart can become enlarged to make up for its limited function.
A baby may be born with just one or several heart defects, some of which may need little or no medical treatment even through adulthood. Others are more serious and can endanger the life of the child — either immediately to the newborn, or over time. Early diagnosis and treatment is critical to the lifelong health and well-being of a child born with a congenital heart defect.
Congestive heart failure (CHF) may be a result of CHD because the heart must work harder than usual. CHF is a serious condition in which the overworked heart does not pump blood efficiently. As the heart works harder, metabolism and energy requirements increase. At the same time, blood flow decreases, resulting in small stomach size and slow gut motility.
In addition, the heart’s inefficient pumping causes fluid to back up into the lungs, liver and other organs. Therefore, children with CHF often require fluid restriction and/or a diet low in salt. This makes it difficult to provide the child with adequate energy intake.

“Melia is now 10. She had three surgeries to strengthen her heart when she first arrived home, but has not seen the operating room since! She gets annual checkups with her cardiologist, but has not needed any further interventions or medications.”
— Katie and Ryan Horner, parents of Melia, who was born with congenital heart disease
Down Syndrome & General Low Tone
Down syndrome, also called Trisomy 21, is a condition in which extra genetic material causes delays in the way a child develops, both mentally and physically.
Medical problems may vary from child to child. While some children diagnosed with need a lot of medical attention, others lead lives where the disease has less of an impact on their daily functions.
Low muscle tone, or hypotonia, is common in kids with Down syndrome, but is less obvious as they get older. Children will reach developmental milestones, like sitting up, crawling, and walking, though typically later than other kids do. Low muscle tone may also contribute to sucking and feeding problems during early childhood, as well as gastroesophageal reflux and constipation.
Fortunately, the health problems associated with Down syndrome can be managed well, especially when detected early, and many resources are available to help children and their families.

“We strongly encourage other families to not shy away from special needs adoption! What you don’t know or understand, you will learn. What fears you have will be erased when you pray and seek the support of others, especially those who have made a similar journey.”
— Jade and David Presnell, parents of Micah, who has Down syndrome
Epilepsy
Epilepsy is considered a disorder of the brain or temporary cerebral dysfunction causing seizures.
Pediatric epilepsy is the most common childhood brain disorder in the U.S., affecting about 470,000 children, according to the American Academy of Pediatrics.
Seizures happen when there is a sudden change in electrical activity in the brain. There are many different types of seizures, and each affects people differently. A child who is having a seizure may stare, collapse, shake or become unaware of what’s going on around them.
Epilepsy in children can be caused by many different health problems like genetic disorders, brain injuries, strokes or brain tumors that change the structure or function of the brain. However, physicians often cannot find the reason why a child develops epilepsy.
Epilepsy affects every child differently depending on their age, the type of seizures they have and how they respond to treatment. Some children can easily keep their seizures under control by taking medication and may outgrow them. Others may have cases that are more difficult to manage and require lifelong treatment.

“We are just astounded by what stimulation and constant love and nutrition is doing. Anna has started to open up like a delightful flower.”
— Amanda Abuhl, mother of Anna, who was born with a rare form of epilepsy
Fetal Alcohol Spectrum Disorder
Fetal alcohol spectrum disorder (FASD) is an umbrella term to describe a broad range of physical, developmental and behavioral conditions that can occur in a child with prenatal exposure to alcohol.
Some children born with FASD may struggle with memory and attention span, communication and language comprehension, hyperactivity, impulsivity and other behaviors. Other children experience mild to no symptoms at all.
There is no cure for FASD, but many things can help children reach their full potential, especially if FASD is identified early.
Families who adopt a child with FASD have found great success by brainstorming ways to help their child and address their behaviors. It is also important for families to have access to FASD-competent therapeutic attention resources, as many children with FASD are misdiagnosed with ADD, ADHD and other disorders.

“FASD seems huge, and there are so many things to prepare for. But when we broke it down into those small aspects to prepare for, some didn’t seem big. But others did, and that’s what we focused on.”
— Cassie Brooks, mother of Emma, who had prenatal exposure to alcohol
Global Developmental Delays
The term global developmental delays, or GDD, is used when a child shows delays across several areas of development, including activities of daily living, learning skills, fine and gross motor skills, personal development, speech and language development, and socialization skills.
Children are typically assessed as having GDD when they are younger than 5 years of age, and when they have delays in two or more diagnostic areas. According to the American Academy of Neurology, GDD affects 1%-3% of children under age 5.
Children with GDD are not labeled as having an intellectual disability because with support at a young age, there is the possibility of adaptive and cognitive development. To assess whether a child has GDD, a pediatrician will analyze your child’s growth chart, perform hearing and vision assessments, conduct genetic tests or blood tests and more.
The pediatrician can then refer your family to a specialist, such as a speech therapist, occupational therapist, physical therapist, developmental specialist and/or dietitian who will work with your child as needed.

“As I experienced life with [my son] and got to know him, I realized on the inside he was the same as me. He was born with a heart to feel and a mind to think. He was born with challenges and strengths, just like me.”
— Jen Skipper, whose son has developmental delays
Human Immunodeficiency Virus
Human immunodeficiency virus (HIV) is the virus that causes AIDS. When a person becomes infected with HIV, the virus attacks and weakens the immune system. As the immune system weakens, the person is at risk of getting life-threatening infections. When that happens, the illness is called AIDS.
HIV can be transmitted to a fetus or newborn during pregnancy, labor, delivery or breastfeeding. However, children born to HIV-positive mothers may not always become infected themselves.
In the U.S., babies born to HIV-positive mothers can receive a test for HIV antibodies at 18 months of age because they still might have maternal HIV antibodies in their system. Alternatively, they can receive two HIV PCR tests, beginning 28 days after birth. One of these tests should be completed after an infant is at least 4 months old to confirm their HIV status.
Children who are HIV positive ideally begin antiretroviral therapy (ART) within the first months of life. These medicines stop the virus from multiplying. Some children diagnosed with HIV later in childhood or who have not received treatment until later in life may experience complications related to their HIV infection. Without treatment, a child’s immune system weakens over time, and infections that are uncommon in healthy children may develop.
However, the prognosis for children with access to specialized HIV treatment is good. These children may lead a normal life when taking ART medications daily, as prescribed, similar to others with chronic illnesses. Currently, there is no cure for HIV, although some progress is being made.

“For now, HIV is little more than a byline in our busy, fun-filled, joyous, crazy lives. And, with the help of daily medications and great communication, we plan to keep it that way.”
— Anne M. Silas (a pseudonym), mother of two children with HIV
Hydrocephalus
Hydrocephalus is the buildup of cerebrospinal fluid around the brain. This accumulation of fluid can result in increased pressure on the brain if it is not properly drained or cleared.
Most children with hydrocephalus will need a shunt, a small plastic tube that is surgically placed in the brain. A shunt helps drain cerebrospinal fluid and redirect it to another location in the body where it can be reabsorbed. This process reduces pressure on the brain.
Many adopted children may not have received a shunt as early as they should have, as this procedure is not always available in all countries. These children often have some damage from pressure on the brain, although they can experience some recovery with treatment. Early intervention will result in better outcomes for children.
Intellectual Disability
Intellectual disability is a term used when there are limits to a person’s ability to learn at an expected level and function in daily life.
Children with intellectual disability might have a hard time letting others know their wants and needs and taking care of themselves.
Intellectual disability could cause a child to learn and develop more slowly than other children of the same age. It could take longer for a child with intellectual disability to learn to speak, walk, dress or eat without help, and they could have trouble learning in school.
Intellectual disability can be caused by a problem that starts any time before a child turns 18 — or even before birth. It can be caused by injury, disease or a problem in the brain.
For many children, the cause of their intellectual disability is not known. However, some of the most common known causes — like Down syndrome, fetal alcohol syndrome, genetic conditions, birth defects and infections — happen before birth. Others happen while a baby is being born or soon after birth. Still other causes of intellectual disability, including serious head injury, stroke or certain infections, occur when a child is older.
There’s no way to cure or treat intellectual disability directly. But with good treatment, children with intellectual disability can have a good quality of life. Treatments focus on helping with adaptive (or learned) behaviors and life skills.

“You can do hard things for the people you love. You can modify your home, your schedule, your wallet, your priorities and your plans. Life is much richer when you aren’t at the center!”
— Amanda Kick, parent of Haddie, who was born with no cerebellum in her brain
Kidney Impairment
Kidneys are important organs in the body that help to process and remove waste and water from the blood, produce urine and regulate electrolytes. Some children can have kidney malformations or impairments or a diagnosed kidney disease.
They may have a kidney that is not working properly, a kidney that has an abnormal anatomy or fluid buildup in the kidney.
Health care professionals may use a urine test, blood test, imaging test, kidney biopsy and/or genetic test to diagnose kidney impairment or disease.
Pediatric nephrologists or pediatric urologists will treat kidney problems in children by first treating or controlling any underlying conditions that may be causing the kidney damage. They may perform surgery to correct a blockage in the urinary tract or prescribe antibiotics to treat an infection.
Some children with acute kidney injury may need dialysis — treatment to filter wastes and extra fluids from the blood — for a short time while their kidneys recover.
When a child’s kidney disease is chronic, or long-lasting, treatment may slow the progression of the disease, ease symptoms and manage complications. Children with severe kidney failure may require a kidney transplant.

“Oftentimes, the label ‘special needs’ means a child needs medical attention that they can’t or won’t receive growing up in an orphanage overseas. It does not always mean an overwhelming, life-consuming issue.”
— Koni Maat, mother of Jing, who was born with kidney impairment
Low Birth Weight
Low birth weight is defined as a birth weight of less than 5 pounds, 8 ounces. Some babies with low birth weight are healthy, even though they’re small. But having a low weight at birth can cause serious health problems for some children.
A baby who is very small at birth may have trouble eating, gaining weight and fighting off infections. Some may have long-term health problems as well.
One of the main causes of low birth weight is preterm birth, meaning the baby is born before 37 weeks of gestation, or pregnancy. Another cause is fetal growth restriction. This occurs when a baby doesn’t gain the weight they should before they are born.
Fetal growth restriction can be caused by many factors. For example, a mother may have an infection or chronic health condition, such as diabetes or a heart, lung or kidney problem. She may lack good nutrition and not gain enough weight during pregnancy. Or the mother may smoke, drink or use drugs while pregnant.
Children who are born at low birth weight should have regular checkups with their pediatrician. These medical visits can help your child’s doctor spot — and address — health conditions and developmental issues that may cause problems as your child gets older.

“[Desmond was] born prematurely at only two pounds and had already faced myriad health issues… [But] the wonderful thing about God’s destiny is that when we walk in His perfect plan for us, we are not limited by our feeble, human abilities. In our weakness, He is strong.”
— Mandie Hickenbottom-Conner, mother to Desmond, born with low birth weight
Microcephaly
Microcephaly is a condition where a baby’s head is much smaller in size compared to other babies of the same age and sex. Head size is an important measurement in monitoring a child’s brain growth.
During pregnancy, a baby’s head grows because the baby’s brain grows. Microcephaly can occur because a baby’s brain has not developed properly during pregnancy or has stopped growing after birth, which results in a smaller head size. Microcephaly can be an isolated condition, meaning that it can occur with no other major birth defects, or it can occur in combination with other major birth defects.
It is a rare condition that can be a symptom of several disorders, including Down syndrome, Rett syndrome and trisomy 18.
Children with microcephaly generally have varying degrees of intellectual disability, though a small percentage will not experience any developmental delays. Children with this condition may also have delayed speech and motor functions, dwarfism or short stature, vision and hearing deficiencies and/or other problems associated with neurological abnormalities.
Developmental services early in life will often help children with microcephaly to improve and maximize their physical and intellectual abilities. These services known as early intervention can include speech, occupational and physical therapies.
Prematurity
A baby born before 37 weeks gestation is considered premature. Slightly less than 12% of all babies are born prematurely.
However, the rate of premature births is rising, mainly due to the large number of multiple births in recent years. Twins and other multiples are about six times more likely than single-birth babies to be born prematurely, although the rate of premature single births is also slightly increasing each year.
A typical pregnancy lasts about 40 weeks, and a developing baby goes through important growth throughout pregnancy, including in the final months and weeks. For example, the brain, lungs and liver need the final weeks of pregnancy to fully develop.
Not all premature babies have health complications. But being born too early can cause short-term and long-term medical problems. Some problems may be clear at birth, while others may not show up until later in life.
In general, the earlier a baby is born, the higher the risk of complications. Birth weight plays a key role too. Many premature babies weigh less than 5 pounds, 8 ounces and may be referred to as low birth weight. Other terms often used for prematurity are preterm or “preemie.”

“As for being totally dependent on us, let’s just say ‘NOT!’ Samuel was a spitfire from day one! ‘I can do it!’ has always been his attitude.”
— Rebecca Tyler, mother of Samuel, who was born prematurely without hands or feet
Prenatal Substance Exposure
Prenatal substance exposure occurs when a mother takes drugs or alcohol while pregnant. Just as nutrition passes from mother to baby, so can toxins from illicit drug use.
Each substance can have its own measurable impact on the development of the fetus, and prenatal exposure can potentially have a negative impact on neural and physical development.
Children can experience both short-term and long-term challenges, including premature birth, low birth weight, birth defects, behavioral and learning issues, sensory system difficulties, increased chance of oral clefts or cleft palate and feeding issues.
Some infants are also born with substance dependency. Short-term withdrawal symptoms may consist only of mild fussiness. More severe symptoms may include irritable or jittery behavior, feeding problems and diarrhea. Symptoms vary depending on which substances were used.

“There’s no doubt about it that he has ‘Hugh quirks’ and we have to parent him differently. But we parent him with all we have.”
— Tara Blackshear, mother of Hugh, who was born with alcohol exposure
Sickle Cell Disease
Sickle cell disease is a group of inherited red blood cell disorders that affect hemoglobin, the protein that carries oxygen through the body.
Red blood cells are normally disc-shaped and flexible enough to move easily through the blood vessels. In sickle cell disease, red blood cells become crescent- or “sickle”-shaped due to a genetic mutation.
These sickled-shaped cells do not bend or move easily and can block the flow of blood to parts of the body. The blocked blood flow can lead to serious problems, including stroke, eye problems, infections and episodes of pain, commonly known as a pain crisis.
Sickle cell disease is a chronic illness, and until recently there were very few treatment options. But early and ongoing medical care and treatment can minimize complications and help children with the disorder lead full and active lives.
Thalassemia
Thalassemia is an inherited blood disorder caused when the body doesn’t produce enough of the hemoglobin protein, which enables red blood cells to carry oxygen.
Some babies show signs and symptoms of thalassemia at birth. Others develop them during the first two years of life.
Thalassemia can cause chronic fatigue, jaundice and anemia. As it progresses, iron in the blood fills the liver or spleen, eventually causing organ failure. Children with untreated thalassemia may be stunted or fail to thrive. Without medical care, their bellies swell and they may lose their teeth.
Thalassemia cannot be cured, but with treatment a child can anticipate a normal life expectancy. Regular blood transfusions and medication can help manage symptoms. In more severe cases, a stem cell transplant can eliminate the need for lifelong blood transfusions and drugs to control the buildup of iron in the bloodstream.
Vision Impairment
Vision impairment refers to any eye condition that inhibits vision, including low vision, vision loss and blindness. Blindness is a severe vision impairment causing a total or near total lack of vision.
Vision impairment can be caused by damage to the eye itself, by the eye being shaped incorrectly or even by a problem in the brain. Some common causes include genetic or neurological conditions, illness, infections, improper eye development, physical damage or vitamin A deficiency.
Children with vision impairment or blindness may experience challenges in terms of their cognitive, physical, emotional and/or neurological growth and development. They may also have feeding challenges.
But treating vision problems early in childhood may protect your child’s sight, and teaching children with severe vision loss how to function as early as possible can help them reach their full potential.

“It was actually very daunting for us. But [my husband and I] just both really felt like [Levi] was supposed to be with our family — so we took a leap of faith.”
— Melissa Combs, mother of Levi, who was born with congenital glaucoma

Check out additional parenting resources!
View our expanded list of recommended parenting websites, books and other resources organized by topic.

